Aug. 18, 2021
A multi-disciplinary team approach to navigating the pathways of lupus disease

When Christine Sperling started experiencing severe joint pain, extreme fatigue, unexplained bruising and developed a rash, she knew something was wrong. After several tests, she was diagnosed with systemic lupus erythematosus (SLE), an autoimmune disease that causes inflammation and can affect any organ in the body.
Thirty years after her diagnosis, Sperling admits that even with treatment options to manage symptoms, living with lupus is unpredictable and challenging.
“Lupus is always on my mind. Even when my disease is stable, I can experience a flare-up that is out of my control,” she explains. “A lupus diagnosis is pervasive through all aspects of my life and something that I will always have to manage as there is no cure.”

Christine and her daughter participated in the Step Out For Lupus - Walk/Run fundraiser in 2018, organized by the Lupus Society of Alberta.
Christine Sperling
Sperling feels fortunate to have a support system and she has witnessed improvements to patient care throughout her journey with lupus.
“My hope for the future is that one day there is no lupus. But in getting there, I hope for continued improvement in disease management, treatments and ultimately a higher quality of life for lupus patients.”
A team of McCaig Institute researchers share the same hope and are working together to improve diagnosis, treatment and management of the disease. By combining expertise in clinical research and basic science studying biomarkers (measurable biological indicators of disease) the team is advancing lupus research and improving patient care.
Multi-disciplinary approach to care and research
When Dr. Ann Clarke, MD, MSc, started at the University in Calgary in 2013, she sparked collaboration in lupus research and care by establishing the University of Calgary Lupus Centre of Excellence in the Cumming School of Medicine. The multi-disciplinary research and care environment combines the expertise of rheumatologists, immunologists, hematologists, nephrologists, and maternal-fetal medicine specialists to advance lupus research and design patient-centered treatment strategies. The team includes researchers, Dr. Marvin Fritzler, PhD, MD, and Dr. May Choi, MD, who help bridge laboratory diagnostics research to clinical outcomes for lupus.
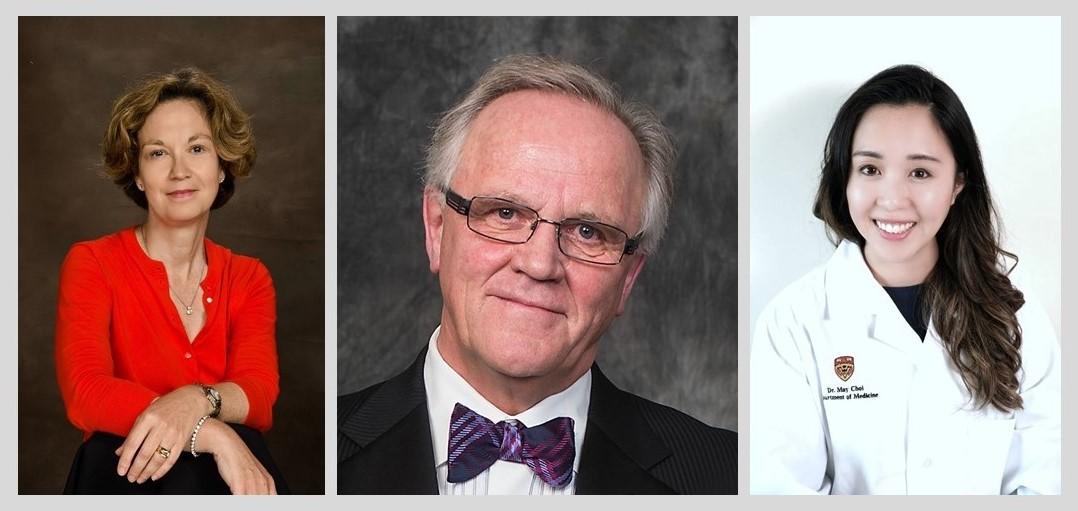
From left, Ann Clarke, Marvin Fritzler and May Choi.
“Because lupus presents in different ways and can cause a wide variety of outcomes, a multi-disciplinary team approach to care and research is needed. The approach offers people living with lupus personalized medicine and the opportunity to participate in clinical trials,” says Clarke.
With the goal of developing new treatments, the team has formed a clinical trial platform to provide patients with early access to specialized and novel therapies.
“Given the spectrum of lupus disease features, we use antibody profiles to identify types of patients who might respond best to new drug therapies. By using a personalized medicine approach, we can offer therapies that effectively control lupus activity with minimal side effects,” explains Clarke.
With interests in the epidemiology of lupus, Clarke’s current research focuses on thrombosis (blood clots), pregnancy complications, and malignancy in lupus and the long-term socio-economic burden associated with lupus. Through her clinical research, she monitors disease features experienced by patients to predict outcomes and improve treatment.
Tracking antibody clues
By combining Clarke’s knowledge of clinical features with the diagnostic expertise of Fritzler and Choi, the team can study the role of antibody biomarkers and their connection with certain lupus disease features.
Fritzler, a world-renowned researcher in the diagnosis of autoimmune diseases, has played an integral role in the University of Calgary’s heritage of lupus research. In 1986, Fritzler developed the Mitogen Diagnostics Laboratory (MitogenDx), which specializes in identifying antibodies and biomarkers for autoimmune diseases. Throughout his career, he has discovered several unique antibodies, leading to breakthroughs in diagnostic testing and an increased understanding of the role of antibodies. With new research approaches, the team continues to re-examine old antibodies and discover new ones to determine their role in predicting disease pathways.
To understand the lupus patient journey Clarke developed a lupus cohort called the Southern Alberta Registry for Lupus Erythematosus (STARLET). The registry has over 400 patients and helps recruit patients into various research studies. When an interested patient joins the registry, the patient's blood is collected and stored in a biobank (freezer) at MitogenDx, and then the detective teamwork begins.
“Identifying specific antibodies that attack a certain part of the cell is important for diagnosing lupus and for predicting disease pathways and outcomes,” explains Fritzler. “Using cohort research in studying antibodies provides evidence of how we can use specific markers to make an earlier diagnosis and monitor disease progression. Early research results show a few disease pathways that a lupus patient will follow, which leads to the question, does a specific antibody mark and predict one of these pathways?”
To better understand the role of antibodies and the progression of lupus, Choi is analyzing data collected from patient registries to monitor the presence of antibodies over time to predict longer-term outcomes of lupus.
Together, the research team is hoping to improve the quality of life of lupus patients by breaking down the complexities of lupus disease and developing a personalized medicine approach to patient care. So that one day, patients like Christine can live pain-free lives without the burden of managing the unpredictability of lupus disease.

Christine Sperling with her son and daughter. She says her family is the most important thing in her life.
Christine Sperling
Dr. Ann Clarke, MD, MSc, is a clinical immunologist and a professor in the departments of Medicine and Community Health Sciences in the Cumming School of Medicine (CSM). She is also the director of the University of Calgary Lupus Centre of Excellence. She is a member of the McCaig Institute for Bone and Joint Health, the O’Brien Institute for Public Health and the Alberta Children’s Hospital Research Institute at the CSM.
Dr. Marvin Fritzler, PhD, MD, is a professor in the departments of Medicine and Biochemistry and Molecular Biology in the CSM and is the Director of MitogenDx. He is a member of both the McCaig Institute for Bone and Joint Health and the Snyder Institute for Chronic Diseases at the CSM.
Dr. May Choi, MD, FRCPC is a rheumatologist and an assistant professor in the Department of Medicine at the CSM. She is the associate director of MitogenDx and the associate director of the Lupus Centre for Excellence and a member of the McCaig Institute for Bone and Joint Health at the CSM.




